Fistulas represent a challenging medical condition where an abnormal tunnel forms between organs or tissues, often causing pain, infection, and discomfort. These passageways can develop in various body areas, but anal fistulas remain among the most common, stemming from untreated abscesses or inflammatory diseases. Cost of laser fistula surgery in Saudi Arabia(تكلفة عملية الناسور بالليزر في السعودية) Patients frequently search for reliable information on when intervention becomes necessary, turning to educational resources for clarity.
This blog dives deep into fistula surgery indications and eligibility, empowering you with knowledge to recognize symptoms early and understand treatment pathways. By exploring causes, diagnostic processes, and candidacy criteria, you'll gain insights that spark informed discussions with healthcare providers. Imagine reclaiming comfort through targeted procedures—let's uncover how.
What Exactly Is a Fistula?
A fistula acts like an unwanted shortcut in your body, connecting spaces that shouldn't link, such as the skin and anus or intestine and bladder. This tunnel often leaks pus, stool, or mucus, leading to relentless itching, swelling, and foul odors that disrupt daily life. Fistula Surgery in Riyadh emerges as a beacon for those in the region seeking advanced care, blending global expertise with local accessibility.
Common types include anal, rectovaginal, and enterocutaneous fistulas, each with unique triggers like Crohn's disease, trauma, or infections. Early detection transforms outcomes, preventing chronic issues. Engaging with this knowledge not only educates but motivates proactive health steps, making you feel empowered rather than overwhelmed.
Primary Causes Leading to Fistula Formation
Fistulas don't appear overnight; they brew from underlying issues like perianal abscesses that burst and fail to heal properly. Inflammatory bowel diseases, such as Crohn's, inflame tissues, creating fertile ground for these tunnels. Trauma from surgeries, radiation therapy, or even childbirth can puncture delicate areas, inviting bacterial invasions.
Infections, particularly in diverticulitis or tuberculosis-prone regions, accelerate fistula development by eroding tissue barriers. Lifestyle factors like chronic constipation strain the anal area, weakening defenses. Recognizing these triggers—through vivid stories of patients who ignored early signs—highlights why awareness drives timely action, turning potential crises into manageable journeys.
Key Symptoms Signaling Fistula Surgery Need
Persistent anal pain throbbing like a drumbeat, coupled with pus-draining wounds, screams for attention. Recurrent abscesses that refill despite drainage indicate a deeper fistula network begging for surgical exploration. Fever, chills, and unexplained weight loss join the party, signaling systemic infection.
Bowel movement changes, like incontinence or bloody stools, erode quality of life, making simple tasks daunting. For women, vaginal discharge or urinary issues point to complex fistulas. These symptoms aren't just nuisances—they're urgent calls to assess fistula surgery indications, urging readers to track patterns and seek evaluations before complications escalate.
When Do Indications for Fistula Surgery Arise?
Fistula surgery indications crystallize when conservative treatments fail, such as antibiotics or seton drainage offering only temporary relief. Chronic, symptomatic fistulas persisting over six weeks demand intervention to halt recurrent infections and tissue destruction. High-output fistulas causing malnutrition or severe Crohn's flares tip the scales toward surgery.
Complex fistulas branching like underground rivers, involving sphincters or multiple tracts, rarely heal spontaneously. Patient suffering—measured by pain scales and quality-of-life surveys—guides decisions. This threshold isn't arbitrary; it's a calculated pivot from watching to acting, illustrated by patient testimonials that resonate emotionally.
Comprehensive Diagnostic Process for Eligibility
Diagnosis kicks off with a digital rectal exam, where specialists palpate for tenderness and tracts, evoking a detective's precision. Imaging like MRI or endoanal ultrasound maps fistula anatomy in stunning detail, revealing hidden branches. Endoanal ultrasonography shines with 80-90% accuracy, guiding precise planning.
Fistulography injects contrast for X-ray visuals, while CT scans rule out abscesses. Exam under anesthesia (EUA) combines diagnosis and initial treatment, probing tracts directly. These steps ensure eligibility by confirming fistula presence, type, and sphincter involvement, building trust through transparent, tech-driven insights.
Advanced Imaging Techniques Explained
MRI fistulography stands out for its non-invasive 3D mapping, color-coding tracts for surgeons. Endoscopic ultrasound probes deliver real-time views, minimizing guesswork. Hydrogen peroxide-enhanced ultrasound bubbles highlight paths vividly.
These innovations reduce recurrence risks, making eligibility assessments sharper and more reliable.
Eligibility Criteria: Who Qualifies for Fistula Surgery?
Prime candidates include adults with confirmed, symptomatic fistulas unresponsive to meds. Good overall health—stable BMI, no uncontrolled diabetes—boosts success odds. Sphincter-preserving eligibility hinges on low fistulas avoiding muscle damage.
Contraindications like active pelvic sepsis or poor wound healing exclude some, prioritizing safety. Age isn't a barrier; fit elderly patients thrive post-op. Pediatric cases, often Crohn's-linked, require tailored evaluations. This criteria demystifies access, reassuring readers they're not alone in the process.
Health and Lifestyle Factors Influencing Candidacy
Smoking cessation enhances healing; quitting months prior slashes complications. Nutritional status, bolstered by protein-rich diets, fortifies tissues. Comorbidities like obesity demand optimization through weight management.
Mental readiness, supported by counseling, correlates with better adherence.
Types of Fistula Surgery Procedures Available
Fistulotomy slices open simple tracts for healing, ideal for superficial cases with minimal sphincter risk. Seton placement threads a band to drain and mature fistulas gradually. LIFT (Ligation of Intersphincteric Fistula Tract) seals internals without cutting externals, preserving continence.
Advancement flaps cover defects with healthy tissue, while VAAFT (Video-Assisted Anal Fistula Treatment) uses scopes for precision. Bioprosthetic plugs fill voids naturally. Each matches fistula surgery eligibility, offering tailored paths to relief.
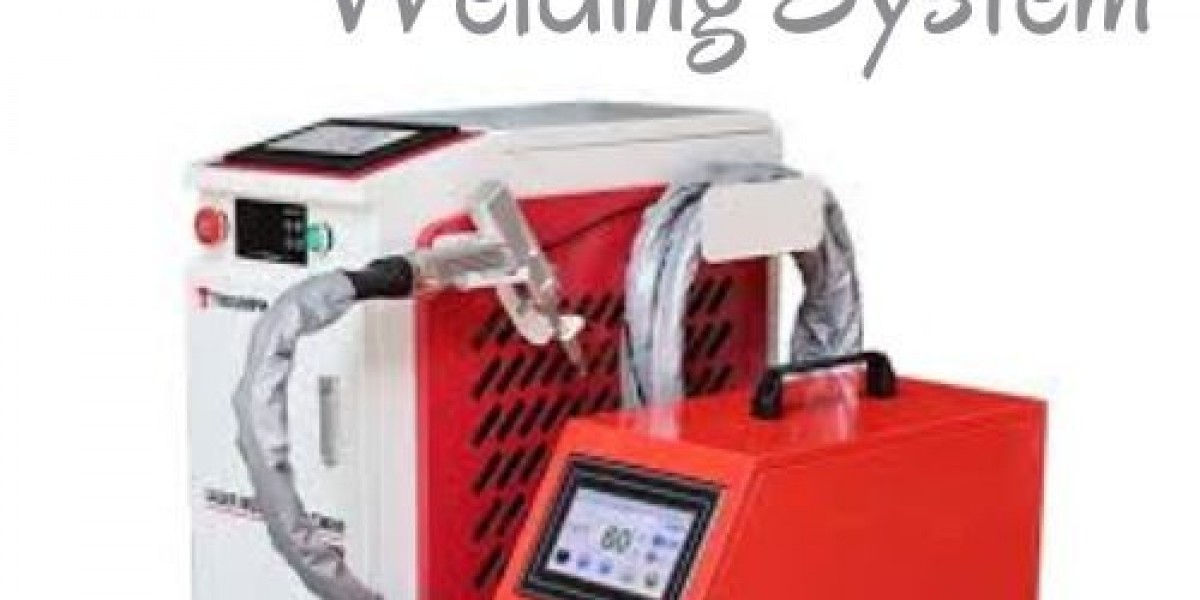
Minimally Invasive Options Gaining Popularity
Laser ablation vaporizes tracts with heat, minimizing bleeding. Fibrin glue seals low-risk fistulas non-surgically. These spark interest with quicker recoveries, drawing clicks from recovery-focused searchers.
Risks, Benefits, and Realistic Expectations
Benefits dazzle: 70-95% success rates heal fistulas, slashing infections and pain. Improved continence and bowel control restore normalcy. Risks like incontinence (5-10% in complex cases) or recurrence demand honest talks.
Infections or bleeding occur rarely with modern techniques. Expectations set via animations show healing arcs, keeping readers hooked on transformative potential.
Preparing for Your Fistula Surgery Journey
Pre-op bowel prep clears paths with enemas and laxatives. Fasting and medication reviews ensure smoothness. Lifestyle tweaks—hydration, light walks—prime the body.
Mental prep via meditation apps eases nerves, turning anxiety into anticipation.
Post-Surgery Recovery Roadmap
Hospital stays last 1-3 days; sitz baths soothe wounds thrice daily. High-fiber diets prevent constipation, with pain meds easing discomfort. Activity ramps up gradually—walking day one, avoiding lifts for weeks.
Wound checks monitor healing; follow-ups track progress. Vivid timelines illustrate milestones, engaging users visually.
Prevention Strategies to Avoid Future Fistulas
Treat abscesses promptly to nip tunnels in buds. Manage IBD with meds and diets. Hygiene rituals and fiber intake fortify anal health.
Regular check-ups catch issues early, weaving prevention into daily habits seamlessly.
Book an Appointment for Consultation
Ready to explore your fistula surgery indications? Book an appointment for a personalized consultation at Enfield Royal Riyadh (إنفيلد رويال الرياض) today. Our expert team guides you through eligibility and next steps with compassion and precision.
FAQs
What are the main fistula surgery indications?
Indications include persistent symptoms like pain, drainage, and recurrent infections unresponsive to non-surgical treatments.
How is eligibility for fistula surgery determined?
Through exams, imaging like MRI, and health assessments ensuring low risks and high success potential.
Can everyone qualify for fistula surgery in Riyadh?
Most symptomatic patients do, barring active infections or severe comorbidities; evaluations personalize decisions.
What recovery time follows fistula surgery?
Typically 4-6 weeks for full healing, with minimally invasive options faster and less painful.
Are there non-surgical alternatives to fistula surgery?
Yes, like setons or glue for simple cases, but surgery offers definitive cures for complex fistulas.