Low white blood cell count, medically known as leukopenia, is a condition where the number of white blood cells (WBCs) in the bloodstream drops below normal levels. WBCs, or leukocytes, play a vital role in the body's immune system, helping to fight off infections, bacteria, viruses, and other foreign invaders.
A normal WBC count typically ranges from 4,500 to 11,000 cells per microliter of blood, though this can vary slightly based on age, sex, and overall health. When the count falls below 4,000, it's considered low, and if it dips under 1,000, it becomes a serious concern, increasing the risk of severe infections. Leukopenia itself isn't a disease but a symptom of an underlying issue, and understanding its causes is essential for proper diagnosis and management.
In adults, low WBC counts can stem from a wide array of factors, ranging from temporary infections to chronic diseases and lifestyle influences. This article explores the primary causes in detail, drawing from medical insights to provide a comprehensive overview. We'll also touch on symptoms, diagnosis, treatment options, and prevention strategies to give a well-rounded perspective on this condition.
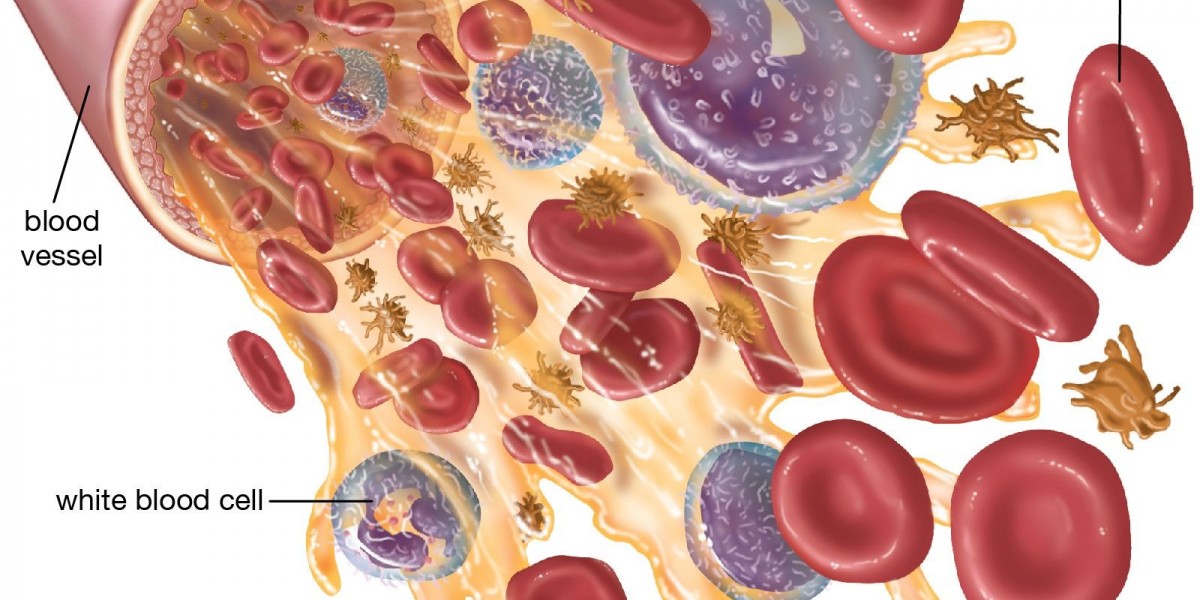
Understanding White Blood Cells and Their Role
Before diving into causes, it's helpful to break down the types of WBCs affected. There are five main types: neutrophils (which fight bacterial infections), lymphocytes (key for viral defense and immunity), monocytes (which handle chronic infections), eosinophils (involved in allergic responses and parasite control), and basophils (related to inflammation). Leukopenia can affect one or more of these, with neutropenia a low neutrophil count being the most common subtype in adults. This distinction matters because different causes target specific WBC types.
Major Causes of Low White Blood Cell Counts
The causes of leukopenia in adults can be categorized into several groups: infections, medications and treatments, bone marrow disorders, autoimmune conditions, nutritional deficiencies, and other miscellaneous factors. Each can disrupt WBC production in the bone marrow, accelerate their destruction, or trap them in organs like the spleen.
Infections
One of the most common triggers for low WBC counts is infection, particularly viral ones that overwhelm the immune system or directly suppress bone marrow function. For instance, viruses like Epstein-Barr (which causes mononucleosis), hepatitis A or B, and HIV/AIDS can lead to temporary or chronic leukopenia by attacking bone marrow cells or causing widespread inflammation.
Bacterial infections, such as tuberculosis, typhoid fever, or severe sepsis, can also deplete WBCs as the body uses them up rapidly to combat the invaders. In overwhelming infections, the bone marrow may not keep up with demand, resulting in a drop. Parasitic infections like malaria can have similar effects by invading red blood cells and indirectly impacting WBC production. While these are often reversible once the infection clears, chronic cases like untreated HIV can lead to persistent low counts.
Medications and Cancer Treatments
Many drugs and therapies interfere with bone marrow activity, making this a leading cause in adults undergoing medical interventions. Chemotherapy and radiation therapy for cancers are notorious for causing leukopenia, as they target rapidly dividing cells, including those in the bone marrow. These treatments can reduce WBC counts significantly, often requiring supportive care to prevent infections.
Other medications, such as antipsychotics (e.g., clozapine), anticonvulsants, and certain antibiotics, can also induce low counts. For example, ceftriaxone, a commonly used antibiotic for bacterial infections, has been linked to rare cases of neutropenia or agranulocytosis, a severe form of low neutrophil count. This side effect occurs through immune-mediated mechanisms where the drug triggers the body to destroy its own WBCs.
Ceftriaxone injection distributors play a role in supplying this medication globally, ensuring it's available for treating conditions like pneumonia or meningitis, but patients on prolonged courses should be monitored for hematologic changes. Additionally, drugs for overactive thyroid or even some over-the-counter pain relievers can contribute if used excessively.
Bone Marrow Disorders
Issues directly affecting the bone marrow, where WBCs are produced, are serious culprits. Aplastic anemia, a condition where the bone marrow fails to produce enough blood cells, often leads to leukopenia and can be triggered by toxins, radiation, or unknown factors. Blood cancers like leukemia or lymphoma invade the bone marrow, crowding out healthy cells and causing low counts. Myelodysplastic syndromes (MDS) and myelofibrosis, where abnormal cell growth or scarring occurs, also disrupt production. These disorders are more common in older adults and often require specialized treatment.
Autoimmune Conditions
In autoimmune diseases, the body's immune system mistakenly attacks its own tissues, including WBCs or bone marrow. Systemic lupus erythematosus (SLE) and rheumatoid arthritis are prime examples, where inflammation leads to increased WBC destruction. Other conditions like Sjögren's syndrome or vasculitis can have similar effects. These are chronic and may fluctuate, with flares causing noticeable drops in WBC counts.
Nutritional Deficiencies
Poor nutrition can impair bone marrow function. Deficiencies in vitamin B12, folate, or copper are linked to low WBC counts, as these nutrients are essential for cell production. This is more prevalent in adults with alcoholism, malabsorption issues (e.g., celiac disease), or restrictive diets. Correcting the deficiency often reverses the leukopenia.
Other Factors
An overactive spleen (hypersplenism) can trap and destroy WBCs, common in liver diseases like cirrhosis. Toxins, such as benzene exposure or heavy alcohol use, can damage bone marrow. Rarely, congenital disorders like cyclic neutropenia appear in adulthood, though they're usually diagnosed earlier. Stress, smoking, and aging can also contribute mildly.
Symptoms and When to Seek Help
Leukopenia often goes unnoticed until an infection arises, as the body struggles to fight it off. Common symptoms include frequent or severe infections, fever, chills, fatigue, mouth sores, and swollen glands. In severe cases, it can lead to life-threatening sepsis. Adults experiencing unexplained infections or persistent tiredness should consult a doctor promptly.
Diagnosis
Diagnosing low WBC counts starts with a complete blood count (CBC) test, which measures WBC levels and subtypes. If low, further tests like bone marrow biopsy, viral screenings, or autoimmune panels may be needed to pinpoint the cause. Imaging or nutritional assessments can also help.
Treatment Options
Treatment focuses on addressing the root cause. For infections, antibiotics or antivirals are used; in medication-induced cases, switching drugs or stopping the offender (like ceftriaxone if implicated) is key. Growth factors like granulocyte colony-stimulating factor (G-CSF) can boost WBC production, especially post-chemotherapy. Bone marrow transplants may be necessary for disorders like aplastic anemia. Supportive care includes avoiding crowds, practicing good hygiene, and monitoring counts regularly.
Prevention Strategies
Preventing leukopenia involves minimizing risks: get vaccinated against preventable infections, eat a balanced diet rich in vitamins, avoid unnecessary medications, and quit smoking. For those on chemo or immunosuppressants, regular blood tests and prophylactic antibiotics can help. Awareness of drug side effects, including those from antibiotics supplied by ceftriaxone injection distributors, is crucial for at-risk patients.
In conclusion, low white blood cell counts in adults arise from diverse causes, but early detection and targeted intervention can mitigate risks. If you suspect leukopenia, seek medical advice prompt action can prevent complications and restore immune health. Always consult healthcare professionals for personalized guidance, as this overview is for informational purposes only.